Hyperopia surgery in Paris
Hyperopia, also known as farsightedness or hypermetropia, is a common refractive error affecting approximately 15% of the population. While corrective lenses are often an effective solution, they may not always be sufficient and can be inconvenient. Various surgical options are available to treat hyperopia when glasses or contact lenses are inadequate.
Learn more about other vision issues
Myopia
Astigmatism
Presbyopia
General information on hyperopia
When light rays enter the eye, they are refracted—meaning their direction is altered—by the cornea and the lens, so that the image is normally focused on the surface of the retina. In hyperopic patients, however, the image is formed behind the retinal plane. This can be due to a slightly shorter eyeball or insufficient refractive power of the eye, often when the cornea is not curved enough. Patients with high hyperopia have poor near vision.
Young patients with mild to moderate hyperopia can often see relatively well without glasses. However, this comes at the cost of constant accommodative effort, which frequently leads to visual fatigue and headaches.
Moreover, as people age, the eye’s ability to accommodate decreases, making hyperopia increasingly bothersome.
Surgical correction of hyperopia is an alternative to wearing glasses or contact lenses. Several methods exist: some use a laser beam, while in other cases—especially for high hyperopia—implantation of a lens is preferable. Occasionally, surgery on the natural lens (crystalline lens) may also be performed to correct the refractive error. The choice among these techniques depends on the patient’s age, the degree of hyperopia, and the anatomical characteristics of the eye, which are assessed during the preoperative evaluation.
Find all Dr Rambaud’s videos on his Youtube channel.
@DocteurCamilleRambaud
Laser surgery for hyperopia: LASIK and PRK
Refractive surgery for hyperopia can be performed using laser techniques, mainly LASIK (Laser-Assisted in Situ Keratomileusis) and PRK (Photorefractive Keratectomy). In both cases, an excimer laser is used to reshape the curvature of the cornea, thereby altering its refractive power. The goal is for incoming light rays to focus on the retina, rather than behind it. The surgeon works on the stroma, the intermediate layer of the cornea located between the epithelium and the endothelium. These procedures are quick, performed under local anesthesia, and on an outpatient basis.
The choice between LASIK and PRK is made during the preoperative assessment and depends on additional tests, mainly corneal topography.
LASIK for hyperopia
To access the stroma, the surgeon first creates a tiny flap in the corneal epithelium using a femtosecond laser. This flap (the “stromal flap”) is then lifted aside, and the excimer laser is used to reshape the curvature of the cornea by acting on the deeper layers of the stromal tissue. At the end of the procedure, the flap is repositioned.
The entire process takes about fifteen minutes in the operating room. The patient usually leaves with relatively clear vision, which typically returns to normal by the end of the day.
PRK for hyperopia
In PRK, a portion of the corneal epithelium is gently removed manually to access the stroma. The excimer laser then reshapes the cornea, but the intervention is less deep than with LASIK.
The epithelium must then heal, resulting in mild to moderate discomfort for about two days. Visual recovery is progressive during the first postoperative week.
Phakic intraocular lens surgery
Phakic intraocular lens implantation is mainly intended for patients with high hyperopia who are not candidates for laser surgery. The principle is to insert a lens into the anterior chamber of the eye, between the iris and the natural lens. This implant is made of collamer, a material that is well tolerated and can remain in the eye permanently. The quality of the implant is crucial; STAAR’s ICL phakic lens implants provide all necessary guarantees.
The main advantage of this technique is its reversibility. The implant can be removed if, as the patient ages, cataract surgery becomes necessary.
This is a well-established method with a long track record: the first phakic lens implants were placed in the 1990s, and nearly 200,000 procedures are performed annually worldwide.
Phakic lens implants can correct hyperopia from +0.5 to +10 diopters, and, if necessary, associated astigmatism from 0.5 to 6 diopters.
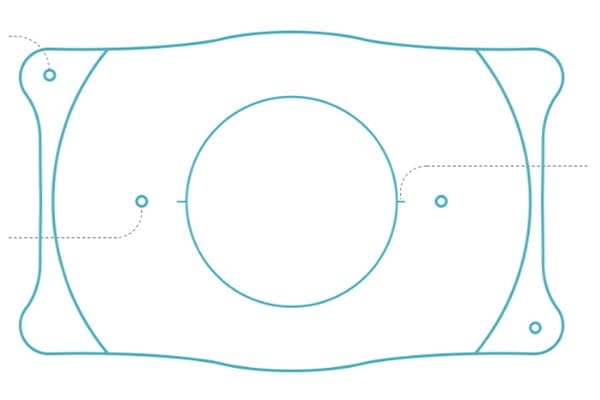
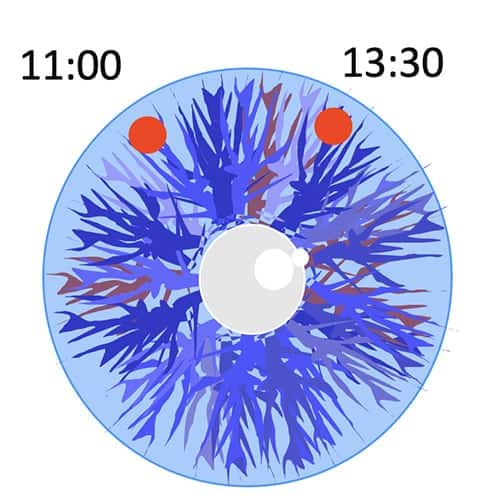
The preoperative process is somewhat more involved than with other refractive surgeries. It includes two laser iridotomies performed a few weeks before the procedure. This involves making two small holes in the peripheral iris, which do not affect vision and ensure proper circulation of the aqueous humor once the implant is in place.
Clear lens extraction surgery
Clear lens extraction is reserved for hyperopic patients over 60 years old. The procedure is similar to cataract surgery: the natural lens is removed and replaced with an artificial intraocular lens. The power of the artificial lens is precisely chosen so that the patient no longer needs glasses after surgery. For hyperopic patients, multifocal implants are preferred, as they allow each eye to see at distance, intermediate, and near ranges.
Frequently asked questions about hyperopia surgery
Does LASIK for hyperopia carry risks?
As with all surgical treatments, there are theoretical risks. The best way to minimize them is to consult an experienced professional equipped with the best technology. If these conditions are met and all contraindications to LASIK are ruled out, complications are very rare and usually consist of infections that respond well to antibiotic treatment.
Although LASIK generally has mild postoperative effects, patients may experience temporary discomfort, such as increased light sensitivity or transient dry eye, which can be managed with artificial tears.
Can laser refractive surgery be performed under general anesthesia for anxious patients?
General anesthesia, even mild, carries more risks than local anesthesia. Moreover, for laser refractive surgery, the patient must be conscious so the surgeon can guide the procedure with the patient’s gaze fixed on a target. If anxiety is significant, it should be discussed with the doctor, who can provide reassurance and explain that the procedure is very brief, with the laser application itself lasting only a few seconds. Modern systems are equipped with safety features, such as eye trackers and automatic laser shutdown in case of excessive eye movement.
Book an appointment with Dr. Rambaud
Have a question? Ask Dr. Rambaud
This page was written by Dr. Camille Rambaud, an ophthalmologist based in Paris and a specialist in refractive surgery.


0 Comments